What is Inflammation? Causes, Types, Symptoms, Treatments, and Support
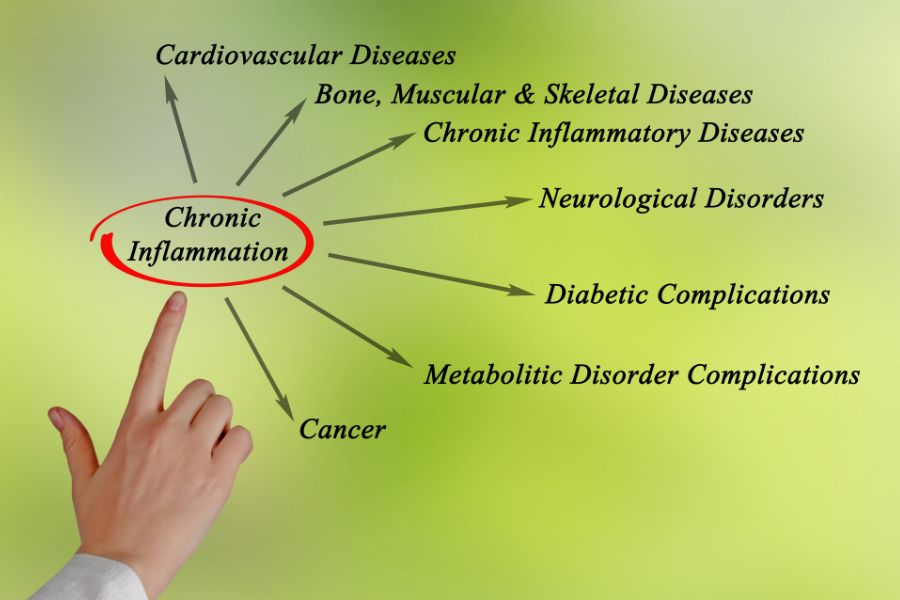
Inflammation is one of the most important yet misunderstood processes in the body. As a natural immune response, it helps fight infections and repair injuries. But when it becomes chronic or widespread, inflammation can damage tissues and contribute to long-term damage and health problems, including arthritis, eczema, gut issues, fatigue, and even mood changes.
This in-depth guide explains everything you need to know about inflammation, based on clinical evidence and UK-relevant health guidance. You’ll learn what causes inflammation, the different types, how to measure it, and what works to reduce it - including diet, supplements, NHS-approved treatments, and realistic lifestyle changes.
Shop anti-inflammatiory supplements

Table of Contents
- What Is Inflammation?
- Types of Inflammation in the Body
- Common Signs and Symptoms of Inflammation
- What Causes Inflammation?
- Testing & Blood Markers for Inflammation
- Foods That Trigger Inflammation
- Anti-Inflammatory Diet
- Inflammation and Genetics
- Hormones and Inflammation
- Inflammation in Older Adults
- Gut and Brain Inflammation
- Skin and Inflammation
- Skincare for Inflammation
- How to Prevent Inflammation
- How to Reduce Inflammation Fast
- Best Supplements for Inflammation
- NHS Treatments for Inflammation
- Inflammation and Long COVID
- Is Inflammation Reversible?
- Summary
- Frequently Asked Questions
- Sources
- Meet the Experts Behind This Guide
What Is Inflammation?
Inflammation is the body’s natural response to stressors like infection, injury, or toxins. It’s part of the healing process but can become problematic when it lingers.
The two main types of inflammation are:
- Acute inflammation: short-term and typically helpful
- Chronic inflammation: low-grade and long-lasting; often harmful
CRP (C-reactive protein) is a key blood marker used to detect both acute and chronic inflammation. It’s produced by the liver and rises quickly in response to injury or infection. Learn more about CRP and other blood tests.
“It’s important to remember that not all inflammation is bad - short-term inflammation helps us heal. The concern is when it becomes invisible and chronic without obvious symptoms.” says Neesha Desai, Pharmacist at Landys Chemist
Types of Inflammation in the Body
- Acute Inflammation: This fast-acting response occurs after injury, infection, or allergic exposure. It causes localised pain, swelling, redness, and heat, and typically resolves in days.
- Chronic Inflammation: Chronic inflammation results from ongoing issues like poor diet, stress, gut imbalance, or autoimmune triggers. Symptoms can include fatigue, joint stiffness, skin flare-ups, and digestive discomfort.
- Systemic Inflammation: Systemic inflammation affects the entire body and is common in autoimmune diseases or chronic metabolic issues. Symptoms often include fatigue, brain fog, aches, or a general sense of being unwell.
- Localised Inflammation: This occurs in specific areas, such as joints (arthritis), gut (IBS), or skin (eczema). Symptoms include pain, stiffness, redness or visible irritation.
Common Signs and Symptoms of Inflammation
- Ongoing tiredness or low mood
- Skin redness or sensitivity
- Joint or muscle pain
- Digestive issues (bloating, diarrhoea)
- Brain fog or sleep disturbance
What Causes Inflammation?
Inflammation is triggered when the body senses damage, infection, or stress. Acute inflammation is usually a direct response to an injury or infection, such as a sprained ankle or bacterial illness - and is often helpful for healing.
However, chronic inflammation is typically driven by longer-term lifestyle and environmental factors that place continued stress on the immune system. Over time, this can disrupt immune balance and contribute to health conditions.
Common causes of inflammation include:
- Injuries and infections: These trigger the short-term inflammatory response needed for repair and immune defence.
- Poor sleep: Less than 6 hours per night is associated with higher CRP levels and disrupted immune signalling.
- Chronic stress: Ongoing stress raises cortisol, which can alter immune function and promote chronic inflammation.
- Obesity and visceral fat: Excess weight, especially around the midsection, produces inflammatory cytokines and disrupts metabolic function.
- Lack of physical activity: A sedentary lifestyle reduces anti-inflammatory immune responses and is associated with higher CRP and TNF-alpha levels.
- Overtraining: Without proper recovery, intense exercise may also raise inflammation markers and delay healing.
- Unbalanced gut microbiome (dysbiosis): Poor microbial diversity can lead to immune system overactivation and inflammation.
- Smoking and tobacco use: These directly damage tissues and increase oxidative stress, fuelling inflammatory processes.
- Alcohol overuse: Excessive alcohol disrupts gut integrity, liver health, and immune balance, all of which can increase inflammation.
- Environmental toxins: Exposure to industrial chemicals, air pollutants, and other toxins can activate immune defences and increase inflammation.
Testing & Blood Markers for Inflammation
Understanding these markers is key to recognising how inflammation shows up in your blood tests. To get any of these tests, including CRP blood tests, you'll typically need to see your GP who will assess your symptoms and refer you for blood testing if appropriate, find out more on the NHS website here
Tests include:
- CRP: A key marker made by the liver. Healthy levels are below 5 mg/L. Raised CRP may suggest infection, injury, or inflammation.
- hs-CRP: A high-sensitivity version of CRP used to detect low-grade inflammation linked to heart health. Below 1 mg/L is ideal.
- ESR: Measures how quickly red blood cells settle in a tube; faster rates suggest inflammation. Often used for monitoring chronic conditions.
- IL-6 and TNF-alpha: Proteins (cytokines) made by immune cells that regulate inflammation. High levels may suggest long-term or systemic immune activity.
Foods That Trigger Inflammation
Certain foods are known to increase inflammation markers:
- Refined sugars and syrups: in fizzy drinks, desserts, sweetened yoghurts
- Fried and processed foods: like chips, crisps, fried chicken
- Trans fats and poor-quality oils: in baked goods, margarine, some snacks
- Processed meats: such as bacon, ham, salami
- Excess alcohol: particularly beer and sugary cocktails
- Additives and emulsifiers in ultra-processed foods (UPFs): found in shelf-stable sauces, instant noodles, and flavoured cereals
Anti-Inflammatory Diet
Diet has one of the most powerful impacts on inflammation. Research suggests that anti-inflammatory diets can reduce CRP levels by up to 25–30% within just a few weeks. Adopting a whole-food, Mediterranean-style approach can significantly improve gut health, immune function, and long-term disease risk.
Studies in Gut and The American Journal of Clinical Nutrition link these diets to lower inflammation, better gut health, and improved immune function.

A well-supported anti-inflammatory diet includes:
- Colourful fruits and vegetables (rich in polyphenols)
- Oily fish (omega-3 sources such as salmon or sardines)
- Whole grains like oats and brown rice
- Extra virgin olive oil
- Nuts, seeds and legumes
- Fermented foods (yoghurt, kefir, sauerkraut)
“A practical tip I give customers is to aim for at least five different colours on your plate, that variety gives your gut and immune system the polyphenols and fibre it needs daily.” — Neesha Desai, Pharmacist at Landy’s Chemist
Inflammation and Genetics
Some inflammatory conditions, such as lupus, Crohn’s, and rheumatoid arthritis, have a hereditary link. However, lifestyle factors usually have a greater impact. A 2020 Nature study confirmed that gut health and daily behaviours play a larger role than genetics alone
Importantly, inflammation risk may begin in pregnancy. Maternal inflammation (due to stress, infection or poor diet) can influence a child’s developing immune system and has been linked to childhood eczema, asthma, and long-term immune challenges.
Hormones and Inflammation
“Hormone-related inflammation can be harder to spot, especially around the menstrual cycle. It’s something I often discuss with women managing endometriosis, where inflammation may contribute to pain and fatigue beyond what’s visible.” says Pharmacist, Neesha Desai
Hormonal changes, especially fluctuations in oestrogen, progesterone, and cortisol - can directly influence inflammation levels. In women, declining oestrogen during menopause is linked to increased inflammation, joint pain, and metabolic changes. High cortisol from chronic stress can suppress immunity and worsen inflammatory conditions. Conditions like PCOS and endometriosis also show evidence of chronic low-grade inflammation.
Studies suggest that balancing blood sugar, managing stress, and supporting hormone health through diet and lifestyle can help reduce inflammation driven by hormonal shifts
Inflammation in Older Adults
Ageing is associated with a gradual increase in low-grade inflammation, often called inflammageing. This is thought to be a key factor in age-related conditions like:
- Cognitive decline
- Frailty and muscle loss
- Cardiovascular issues
Research shows that anti-inflammatory nutrients (like omega-3s, curcumin, and vitamin D), strength training, and maintaining a healthy microbiome can help counteract ‘inflammageing’ and support healthy ageing.
Gut and Brain Inflammation
The gut hosts 70–80% of the immune system. Disruptions to the gut microbiome can trigger inflammation. Fermented foods, fibre, and probiotics can help restore balance.
Neuroinflammation affects mood, focus, and cognition. It's involved in long COVID and conditions like Alzheimer’s and depression. Learn how NADH can help with long Covid symptoms here

Skin and Inflammation
Skin inflammation can appear as redness, itching, swelling, or sensitivity. But these surface symptoms often stem from deeper inflammation inside the body - especially in the gut and immune system.

Conditions like eczema, psoriasis, rosacea, and acne have been linked to raised inflammatory markers and immune imbalance:
- Eczema is triggered by immune overactivity and skin barrier weakness. Research shows that raised cytokines like IL-4 and IL-13 are involved.
- Psoriasis is an autoimmune condition where inflammation causes skin cells to multiply too fast. Curcumin and omega-3s have been shown to reduce flare-ups.
- Rosacea involves vascular inflammation and skin sensitivity. Diet, zinc and quercetin may help calm redness.
A 2020 review in Nutrients found that low vitamin D is associated with skin inflammation, and improving vitamin D status helped reduce flare-ups. Zinc, omega-3 and polyphenols (from plants) may also reduce inflammation affecting the skin.
What’s important to know is that skin symptoms may not just be surface-level - they can reflect broader inflammation happening inside the body, especially from gut issues, chronic stress, or poor diet. Addressing systemic inflammation through nutrition and supplements often leads to clearer, healthier skin.
How Skincare Can Help with Inflammation
Although inflammation often starts from within the body, the right skincare can make a significant difference in calming symptoms and restoring skin health. For conditions like eczema, rosacea, acne, or general sensitivity, topical products can help reduce redness, support the skin barrier, and ease discomfort.
Inflamed skin is often linked to a weakened barrier, overactive immune responses, and disrupted microbiome. Skincare helps by:
- Rebuilding the skin barrier with skincare ingredients like ceramides, hyaluronic acid and niacinamide
- Calming visible redness using soothing ingredients such as oat extract, panthenol and centella asiatica
- Supporting the skin microbiome with gentle cleansers and probiotic formulas
- Reducing oxidative stress with antioxidant-rich serums containing vitamin C or green tea extract
Best Skincare Ingredients for Inflammation
- Ceramides: Help repair the skin’s natural barrier and lock in moisture
- Niacinamide (Vitamin B3): Reduces redness, improves resilience, and supports oil control
- Panthenol (Vitamin B5): Calms and hydrates dry, irritated skin
- Colloidal Oatmeal: Proven to soothe itching and flare-ups, especially in eczema
Centella Asiatica (Cica): A plant extract known for healing and anti-redness benefits - Zinc PCA: Combines calming and oil-regulating properties, ideal for acne-prone skin
Shop from our skincare products by ingredient
Tips for an Anti-Inflammatory Skincare Routine
- Stick to fragrance-free, alcohol-free products
- Use a barrier-repair moisturiser daily, especially after cleansing
- Avoid physical exfoliants or harsh scrubs
- Introduce one new product at a time to track reactions
- Protect your skin with a mineral SPF, especially during flare-ups
Skincare alone won't resolve inflammation, but when used consistently alongside an anti-inflammatory diet, stress management, and the right supplements, it can significantly improve skin comfort and resilience over time.
How to Prevent Inflammation
Preventing inflammation is often more effective than treating it after it becomes chronic. While some inflammation is unavoidable (like that from infections or injury), many lifestyle choices can significantly reduce your long-term risk. Prevention is especially important if you have a family history of autoimmune conditions, cardiovascular disease, or metabolic disorders.
Evidence-backed strategies to prevent inflammation include:
- Follow a diverse, whole-food diet: Emphasise colourful vegetables, healthy fats, fibre, and omega-3s. Avoid ultra-processed foods high in refined oils, additives, and sugar.
- Prioritise sleep: Aim for 7–9 hours of quality sleep per night. Consistent sleep-wake cycles regulate your immune system and reduce CRP levels.
- Exercise regularly: Moderate physical activity (like walking, swimming, or resistance training) can lower inflammatory cytokines. Even 30 minutes a day can help.
- Manage stress daily: Incorporate tools like deep breathing, mindfulness, yoga, or journaling. Reducing cortisol can calm the immune system and reduce low-grade inflammation.
- Avoid smoking and limit alcohol: Both are proven inflammation triggers. Reducing exposure can significantly support immune and cardiovascular health.
- Support your gut: A healthy gut microbiome helps regulate inflammation. Include fermented foods, fibre-rich plants, and consider probiotics if needed.
- Keep a healthy weight: Maintaining a BMI within a healthy range and avoiding visceral fat can significantly reduce long-term inflammation markers.
Long-term prevention is about consistency - not perfection. Small, sustainable changes to how you eat, sleep, move, and handle stress can have a lasting impact on inflammation levels.
How to Reduce Inflammation Fast
If you're dealing with a sudden flare-up - like joint pain, fatigue or skin redness, these fast-acting strategies can help ease inflammation quickly:
- Take NSAIDs: Over-the-counter anti-inflammatories like ibuprofen can provide rapid symptom relief (if suitable for you). Take a look at the NSAID options on the NHS website here
- Apply cold compresses: Ice packs or cool showers help reduce swelling and pain
- Hydrate well: Water supports detox and tissue repair — avoid sugary or alcoholic drinks
- Eat anti-inflammatory foods: Ginger, turmeric, oily fish and berries can help settle inflammation
Prioritise rest: A single night of deep, restorative sleep can calm inflammatory signals
Take a look at when to get medical help for your inflammation here

Best Supplements for Inflammation
These anti-inflammatory supplements are supported by clinical research and may help reduce inflammation in various forms (you can shop here):
- Curcumin (95%): Studies show it can lower inflammation markers and reduce joint pain; one meta-analysis found a significant reduction in CRP and other inflammatory markers with curcumin supplementation.
- Omega-3 (EPA/DHA): Supplementation has been shown to reduce CRP and joint stiffness. Research suggests 2–3g daily is effective for reducing systemic inflammation.
- Magnesium: Clinical trials link low magnesium levels to elevated CRP and chronic stress-related inflammation; supplementation may help normalise these markers.
- Vitamin D: Low vitamin D is consistently associated with increased inflammation. Supplementation supports immune regulation and may reduce flare-ups.
- Boswellia: Research shows it inhibits inflammatory pathways and may significantly reduce joint pain and improve gut health in inflammatory bowel disease.
- Quercetin + Bromelain: Known to support allergy symptoms and gut health. One study found reduced inflammation and improved gut barrier function after 8 weeks of use.
- Resveratrol: Powerful antioxidant shown to reduce oxidative stress and lower inflammation, particularly in skin and cardiovascular health.
- SAMe: Supports joint comfort and liver detoxification. Clinical reviews suggest it may match NSAIDs in improving joint symptoms without their side effects.
- Zinc + Vitamin C: These support tissue repair and immune balance. Studies link zinc deficiency with higher levels of inflammation.
- Alpha-lipoic acid: Reduces inflammation related to blood sugar and nerve health. Clinical trials show improved inflammatory markers and oxidative stress. Take a look at the best ALA supplement for diabetes here.

NHS Treatments for Inflammation
Treatment may involve:
- NSAIDs – such as ibuprofen
- Steroids – oral or topical for severe inflammation
- DMARDs – for autoimmune diseases
- Biologics – injections for immune-related inflammation
- Lifestyle support – dietetics, physio or counselling
Inflammation and Long COVID
Chronic symptoms may be driven by lingering inflammation. Early studies suggest omega-3, vitamin D, magnesium and CoQ10 may support recovery.
Is Inflammation Reversible?
Inflammation can be reversed or managed in many cases. Acute inflammation typically resolves in a few days. Chronic inflammation can improve significantly over weeks or months with targeted diet changes, supplements, physical activity, stress reduction, and medical treatment if needed.
Summary
This guide has explored the key causes, types, symptoms, and proven ways to reduce inflammation, with a focus on practical, evidence-backed solutions. From identifying triggers and improving your diet to supporting your body with the right nutrients, small, consistent changes can have lasting impact.
If you're exploring natural ways to reduce inflammation, supplements like curcumin, omega-3s, and magnesium may offer additional support. For high-quality, clinically researched options, browse our curated range of anti-inflammatory supplements in the UK designed to complement lifestyle and dietary changes.
Taking action early can support your overall wellbeing and help prevent long-term health issues.
Frequently Asked Questions
What is a CRP blood test and what does it show?
CRP (C-reactive protein) is a marker of inflammation measured through a blood test. It shows how much inflammation is present in the body. A CRP level under 5 mg/L is generally considered normal. Higher levels may indicate infection, injury, or chronic inflammatory conditions like arthritis or IBD. To understand more about DRP blood tests visit the NHS website, or a medical information site like Great Ormond Street Hospital
How can I reduce inflammation naturally?
You can reduce inflammation naturally by eating more anti-inflammatory foods (like oily fish, colourful vegetables, and olive oil), improving your sleep, managing stress, staying physically active, and taking supplements such as curcumin, omega-3, and vitamin D. Even small lifestyle changes can make a big difference over time.
What are the symptoms of inflammation in the body?
Symptoms of inflammation can include tiredness, joint or muscle pain, skin redness or sensitivity, digestive issues (like bloating), and brain fog. Chronic inflammation can also affect mood, sleep, and long-term immune health.
Is chronic inflammation reversible?
Yes, in many cases chronic inflammation can be improved or reversed through targeted diet changes, supplements, lifestyle habits, and medical treatment if needed. Unlike acute inflammation, chronic inflammation requires a longer-term approach, but results can be seen within weeks or months.
What foods help lower inflammation?
Foods that help lower inflammation include oily fish (like salmon and mackerel), berries, dark leafy greens, nuts and seeds, olive oil, turmeric, and fermented foods such as kefir or sauerkraut. These foods provide antioxidants, omega-3s, and polyphenols that support immune regulation and tissue repair.
Sources
- C-Reactive Protein (CRP)
- Structural basis for IL-12 and IL-23 receptor sharing reveals a gateway for shaping actions on T versus NK cells
- Sleep Duration and Biomarkers of Inflammation - PMC
- Get help with stress - NHS
- Adipose tissue inflammation and metabolic dysfunction in obesity - PMC
- Inflammatory Effects of High and Moderate Intensity Exercise—A Systematic Review - PMC
- Role of the Microbiota in Immunity and inflammation - PMC
- Air Pollution: Possible Interaction between the Immune and Nervous System? - PMC
- Blood tests - NHS
- Associations between dietary patterns and an array of inflammation biomarkers and plasma lipid profile in postmenopausal women
- Diet quality inversely associated with C-reactive protein levels in urban, low-income African American and White adults
- Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials - PubMed
- Effect of 1-year lifestyle intervention with energy-reduced Mediterranean diet and physical activity promotion on the gut metabolome and microbiota: a randomized clinical trial
- C. elegans interprets bacterial non-coding RNAs to learn pathogenic avoidance | Nature
- Inflammatory Conditions During Pregnancy and Risk of Autism and Other Neurodevelopmental Disorders - ScienceDirect
- Menopause, obesity and inflammation: interactive risk factors for Alzheimer’s disease - PMC
- Chronic low-grade inflammation and ovarian dysfunction in women with polycystic ovarian syndrome, endometriosis, and aging - PubMed
- Hormonal and Metabolic Changes of Aging and the Influence of Lifestyle Modifications - PMC
- Inflamm-ageing: How cytokines and nutrition shape the trajectory of ageing - ScienceDirect
- Anti-Inflammatory Properties of Diet: Role in Healthy Aging - PMC
- Inflammation at the crossroads of COVID-19, cognitive deficits and depression - PMC
- https://www.ncbi.nlm.nih.gov/books/NBK538209/
- Study on the use of omega-3 fatty acids as a therapeutic supplement in treatment of psoriasis
- Vitamin D in the Prevention and Treatment of Inflammatory Skin Diseases - PMC
- NSAIDs - NHS
- Effect of curcumin on rheumatoid arthritis: a systematic review and meta-analysis - PMC
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12079108
- Magnesium deficiency and increased inflammation: current perspectives - PMC
- Boswellia: Usefulness and Safety | NCCIH
- Potential Implications of Citrulline and Quercetin on Gut Functioning of Monogastric Animals and Humans: A Comprehensive Review
- S-Adenosyl methionine (SAMe) versus celecoxib for the treatment of osteoarthritis symptoms: A double-blind cross-over trial. [ISRCTN36233495] - PMC
- Zinc deficiency enhanced inflammatory response by increasing immune cell activation and inducing IL6 promoter demethylation
- A Study to Evaluate the Effect of Alpha-Lipoic Acid on Neuropathic Symptoms in Diabetic Neuropathy Patients on Gabapentin or Pregabalin
- Biologic and Targeted Synthetic DMARDS | North Bristol NHS Trust
- About adalimumab - NHS
- Coenzyme Q10: Clinical Applications beyond Cardiovascular Diseases - PMC
- Understanding your child's blood tests | Great Ormond Street Hospital
Medically Reviewed & Authored By
This article was medically reviewed by Girish Desai, Chief Pharmacist at Landys Chemist since 1982 (GPhC Reg. No. 2019217), with expert clinical input from Neesha Desai, Pharmacist (GPhC Reg. No. 2071387).
Written and compiled by Rhysa Phommachanh, Head of Digital at Landys Chemist and specialist in health and wellbeing content strategy.
This content is grounded in current NHS guidance, clinical research, and expert pharmacy knowledge to ensure accuracy and relevance for UK readers. For personalised advice, always consult your GP or a qualified health professional.